State plans new hospital categories under SHIF to curb fraud

CS Nakhumicha highlighted ongoing investigations into fraudulent claims, revealing that an internal audit directorate examined 31 healthcare providers between July 2022 and December 2023.
The Ministry of Health is set to re-categorise all hospitals before their empanelment by the Social Health Insurance Fund (SHIF).
The move is in a bid to eliminate fraud that has seen taxpayers lose millions of shillings through fictitious claims against the National Health Insurance Fund (NHIF).
Related Stories
Health Cabinet Secretary Susan Nakhumicha made this announcement during a session with the National Assembly’s Health Committee, revealing the plan to involve the Kenya Medical Practitioners and Dentist Council (KMPDC) as the sole body responsible for inspecting and categorising hospitals.
CS Nakhumicha expressed concern about the misclassification of hospitals, stating, "We have found that there are hospitals that are categorised as Level Four when they are Level Two."
She emphasised that this misclassification has allowed certain hospitals to claim funds from the National Health Insurance Fund (NHIF) at rates they are not entitled to.
Under the new Social Health Authority (SHA) Act, the KMPDC will play a crucial role in inspecting, categorising, and licencing hospitals before they can participate in the SHIF for claim payment. The objective is to address the ongoing issue of fraudulent claims and enhance the integrity of the healthcare system.
The Health Act defines six categories of hospitals, ranging from Level One community facilities to Level Six national referral hospitals.
According to KNBS, there are 12,821 Level 2 hospitals, 2,712 Level 3 facilities, 958 Level 4 district hospitals, 20 Level 5 district referral hospitals, and 6 Level 6 national referral hospitals in the current healthcare infrastructure.
Internal audit
CS Nakhumicha highlighted ongoing investigations into fraudulent claims, revealing that an internal audit directorate examined 31 healthcare providers between July 2022 and December 2023.
 Health CS Susan Nakhumicha when she appeared before the National Assembly Departmental Committee on Health on Feb 15, 2024. (Photo: MOH)
Health CS Susan Nakhumicha when she appeared before the National Assembly Departmental Committee on Health on Feb 15, 2024. (Photo: MOH)The investigations uncovered breaches of contractual obligations, leading to recommendations for refunds, stopping payments on claims, and potentially suspending or terminating contracts.
However, Nakhumicha explained that the NHIF board has not yet met to deliberate on these recommendations due to the transition to the Social Health Authority.
During this period, the Attorney General has advised the board to focus solely on winding up the fund during this period.
Health PS Harry Kimtai stressed the importance of accountability under the new law.
"In cases of fraud, the KMPDC will be held accountable. The SHA brings accountability," he said.
He confirmed that no hospital would be empanelled by the SHA without clearance from the KMPDC.
The National Assembly’s Health Committee, chaired by Endebess MP Robert Pukose, recently concluded its inquiry into the collusion between healthcare providers and NHIF officials to defraud the national insurer of millions of shillings.
NHIF CEO Elijah Wachira provided details on fraudulent claims, citing examples such as Beirut Pharmacy and Medical Centre, which submitted 1,706 claims, of which 1,592 were paid, amounting to Sh153.43 million.
"Monitoring conducted at the sampled employers revealed that 26 employees of Employer A were confirmed by the employer to have been at work throughout admission," he said.
As a result, Sh3.65 million in paid claims were identified as fraudulent, and Beirut Pharmacy and Medical Centre were required to repay Sh15.49 million.
The investigation also focused on Amal Hospital, which submitted 504 claims, of which 267 worth Sh34.65 million were paid.
The audit committee recommended that Amal Hospital repay NHIF Sh7.6 million, and claims totalling Sh32.25 million should be rejected. For Joy Nursing and Maternity Hospital, similar recommendations were made to reimburse NHIF Sh73.96 million.
Top Topics This Week
kenya passports
passports backlog kenya
Maisha Card
Immigration Principal Secretary Julius Bitok
passport delays
passport printing kenya
immigration office kenya
1994 Rwandan genocide
rwanda genocide suspects
Charles Sikubwabo rwanda genocide
Ryandikayo rwanda genocide
rwanda genocide fugitives
Patrick Amoth
Sherehe GSM maize flour
aflatoxin maize flour kenya
Gor Mahia
AFC Leopards
Tusker
FKFPL
Kenyan Football
Trending

Mombasa and Embu counties agree to regulate sale of muguka and miraa to minors
Farhiya Hussein
|
20 hours ago

Garissa set to host Northern Frontier's first industrial park as state releases funding
Barack Oduor
|
2 days ago

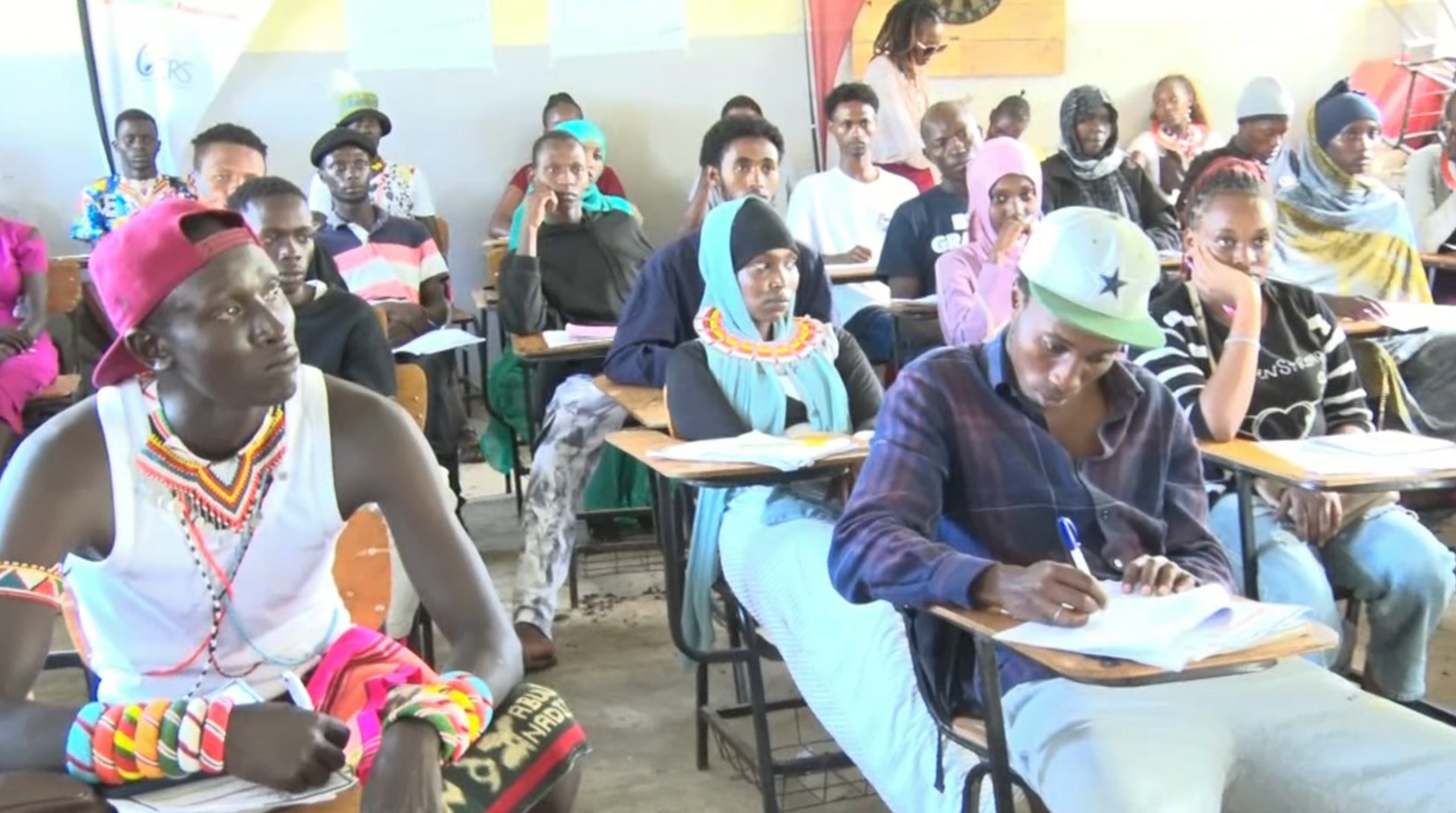
Learners report back to school across the country after floods delay
Eastleigh Voice Team
|
3 days ago

Floods bring blessing for youth harvesting metals from Nairobi River for resale
Abdirahman Khalif
|
1 week ago
EGYPT-UN-PALESTINIAN-ISRAEL-CONFLICT-BORDER-AID
Dennis Tarus
|
6 months ago